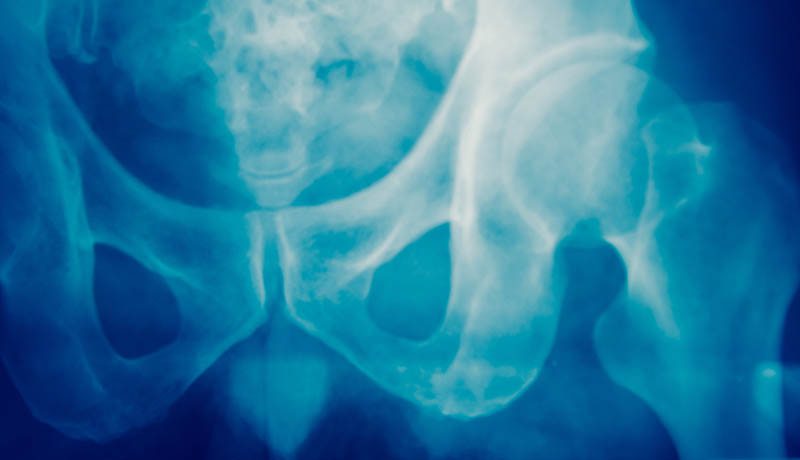
Osteoporosis
Symptoms in Detail
One of the major side effects of menopause can be osteoporosis
- a serious health concern that can have an impact on a woman’s physical health causing chronic pain and broken bones.

What is Osteoporosis?
Osteoporosis (meaning porous bone) is a skeletal disease characterised by weakened bones and increased risk of bone fractures.
Bones are in a constant state of renewal but the process is regulated – among other things – by estrogen and vitamin D3. It’s a condition that’s inextricably linked to our hormones because menopausal estrogen decline mean its role in the turnover of bone is impaired. This culminates in bone loss and low bone mineral density.
The prevalence of osteoporosis is on the increase and affects more than half of women over 60. We lose bone mass two to four times faster after menopause – 10 percent of it in the first five years of post-menopause.
Osteoporosis can also be linked to issues with your gums and teeth such as bone loss post-menopause.
What can you do to help prevent this symptom?
Osteoporosis is believed to run in families and is a ‘silent disease’ so you may not know you have it. Women are far more likely to get osteoporosis than men and growing older is a risk factor. There are some steps you can take to help minimise your risk and the severity of the condition whether or not you have genetic links.
- Get a bone density (DEXA) scan.
- Partake in weight bearing exercise: walking, jogging, tennis.
- Resistance training with weights helps build bone strength.
- Ensure your calcium, magnesium and vitamin D levels are adequate.
- Magnesium helps the body absorb both calcium and vitamin D.
- Eat a diet rich in protein, vitamins C, D, K, calcium, magnesium and zinc.
- Foods high in calcium include seeds, almonds, tofu, soy milk, figs, edamame, kale, broccoli, sweet potato, sardines, salmon and if you can tolerate dairy and lactose cheese, milk and yoghurt.
- Avoid caffeine, salt and alcohol as it inhibits calcium absorption.
- If you smoke stop.
- Take 55+ as it contains EstroG-100™ for hormone balance and the added support of magnesium and vitamin D3.
Osteoporosis: Why Strong Bones Are So Important At Post-Menopause
Today we’re going to talk about bones. And more specifically osteoporosis, because it’s something we all need to know about. Especially if we’re in pre-, peri- or post-menopause. If there’s one thing I’ve learned it’s that many of us are woefully uneducated when it comes to menopause and health. Particularly when it comes to the

6 Things Every Woman Ought To Know About Menopause, Magnesium & MenoMe® 55+
Magnesium. Also known as the ‘mighty mineral’, magnesium is vital to wellbeing which is why we’ve included it in 55+. In this story we’ve given you the lowdown on the magnesium we use in 55+. In addition, we’ve shared why we use marine magnesium. 1. Magnesium deficiency is common Worldwide, many people aren’t getting enough magnesium.
Know the 34 symptoms of menopause
Here are all of the documented symptoms of menopause you need to look out for:
Physical Symptoms
- Incontinence
- Changes in Body Odour
- Bouts of Rapid Heart Beat
- Breast Pain
- Headaches
- Joint Pain
- Itchy Skin
- Burning Mouth Syndrome
- Electric Shock Sensation
- Digestive Problems
- Gum Problems
- Increased Tension in Muscles
- Formication - Crawly Skin
- Paresthesia - Numbness in Hands and Feet
- Osteoporosis - After Several Years






